National Vascular Registry Report 2022: Summary for Anaesthetists
The NVR is commissioned by the Healthcare Quality Improvement Partnership (HQIP) as part of the National Clinical Audit and Patient Outcomes Programme and is designed to promote quality improvement within NHS hospitals performing vascular surgery by providing information on their performance.
In this summary we present data with direct relevance to vascular anaesthetists. The full report is available at https://www.vsqip.org.uk/content/uploads/2022/11/NVR-2022-Annual-Report.pdf
Carotid endarterectomy
In 2021, a total of 3,171 carotid endarterectomies were performed in the UK. This number has increased slightly from 2020, when 3,063 carotid endarterectomies were performed, but this number remains significantly lower from 2019, when 4,162 procedures were performed. This overall 25% reduction in carotid endarterectomies performed in 2020 and 2021 was noted from April 2020 following the impact of the COVID-19 pandemic.
Operative details of unilateral carotid endarterectomies performed during 2021:
- 63.6% were performed under general anaesthesia (GA) alone
- 7.9% were performed under local anaesthetic (LA) alone
- 10.6% were performed under combined GA/LA or block
- 7.99% were performed under block or regional
- 64.2% of procedures involved the use of a shunt
Medication for cardiovascular conditions was common among patients prior to surgery. Overall, 81.2% were taking statins, while 91.5% were on antiplatelet medication (54.9% on single therapy and 45.1% on dual therapy).
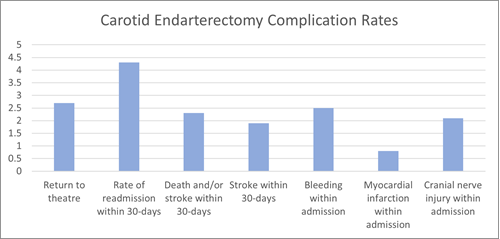
Surgical outcomes continue to be satisfactory with the estimated rates of different complication being 0.5-2.5%. This has remained consistent over the last few NVR annual reports. The median length of hospital stay was 2 days (IQR: 1-5 days).
Areas of improvement highlighted by the report were:
- Time from symptoms to surgery: According to the NICE guideline NG128, the recommended target time from symptom onset to surgery is to be 14 days. The median time from symptom onset to surgery for symptomatic patients in 2021 was 13 days (IQR 8-22 days). The median time delays were:
- 4 days (IQR 1-8) from symptom to first medical referral
- 1 day (IQR 0-4) from first medical referral to being seen by the vascular team, and
- 6 days (IQR 3-9) from being seen by the vascular team to undergoing CEA
There was considerable variation between NHS trusts in the median time to surgery. Forty-four out of the 66 NHS trusts had a median time of 14 days or less. In 4 of the vascular units, the median wait exceeded 20 days, a considerable improvement from 16 units in 2016. Nineteen trusts had less than half of their patients operated on within 14 days.
Major Recommendations:
- Review and improve referral pathways
- Ensure timely referral and expedited surgery for patients with symptomatic carotid disease with measures to reduce waiting times to carotid endarterectomy
Repair of elective infra-renal aortic aneurysms
The organization of vascular services undertaking AAA repair continues to evolve. The number of NHS vascular units performing AAA repairs decreased from 74 in 2019 to 71 in 2021.
There were 2744 elective infra-renal AAA repairs submitted to the NVR in 2021, of which 59% were endovascular repairs and 41% were open repairs. There was an increase in procedures compared to 2328 elective repairs performed in 2020, but numbers are not still back up to the pre- COVID-19 pandemic levels. There is still a large backlog of patients with an AAA waiting for surgery.
In the last decade, there has been a decrease in the proportion of elective AAA repairs performed as endovascular (EVAR) procedures. The reasons for this could be a more conservative approach to treatment (particularly in older, sicker patients) and the influence of the draft NICE guidance, which favoured open repair over an endovascular approach.
However, over the last three years, the proportion of EVAR procedures has been stable, at around 60%. There is a distinct pattern in the numbers of patients having open and endovascular procedures among the age groups, with open repairs being more common among patients aged under 70.
NHS vascular units achieved good patient outcomes after elective infra-renal AAA repair in 2021. Over the 3-year period from January 2019 to December 2021, the risk-adjusted in-hospital mortality rates for all NHS vascular units were within the expected range of the national average (1.4% for 2019-2021).
Postoperative in-hospital mortality after open repair has decreased slightly; in 2021, the rate was 3.1% compared to 3.2% in 2020 respectively. For EVARs, the rate has slightly increased to 0.5% in 2021 compared to 0.3-0.4% in 2020. The very low in-hospital mortality rates following elective EVAR repair raises the question of whether mortality remains the most valuable measure of outcome for infrarenal AAA.
Patients undergoing open repair (OR) were more susceptible to cardiac, renal and respiratory complications, and the rate of return to theatre was also higher. For open repair, the rate of respiratory complications was 10.1% (95% CI 8.4 to 12.0) in 2021, a slight fall from 12.1% (95% CI 10.1 to 14.3) observed in 2020. For EVARs, respiratory complications also decreased from 1.5% (95% CI 0.9 to 2.3) to 1.2% (95% CI 0.8 to 1.9) between 2020 and 2021
Over 70% of elective EVAR went to a standard ward after surgery, while over 95% of patients undergoing OR were admitted to a level 2 or level 3 critical care unit.
The median length of hospital stay was 7 days for OR (IQR 6-10) and 2 days for EVAR (IQR 1-3).
Data is now collected against the standards of the VSGBI Quality Improvement Framework
Overall compliance with standards related to the elective AAA care pathway
(Percentage of patients meeting standard)
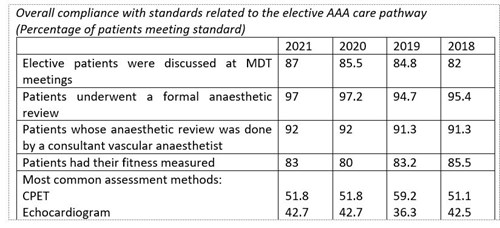
The report also examined the influence of frailty in patients undergoing elective AAA repair. In 2021, frailty was recorded in 72% of patients, a slight decrease from the 76% achieved in 2020. Vascular units were encouraged to identify at risk ‘frail’ patients and ensure their degree of frailty is submitted to the NVR. Therefore, there was insufficient data to demonstrate a relationship between frailty and in-hospital postoperative mortality. From the available data however, there appears to be a higher prevalence of frailty in those having EVAR compared to open repairs.
Complex aneurysm repair
Aneurysms can occur at various locations along the aorta. In addition to infra-renal aneurysms, a distinction is made between three other types, which collectively are referred to as complex aneurysms:
- juxta-renal (that occur near to the renal arteries)
- supra-renal (that occur above the renal arteries)
- thoraco-abdominal (more extensive aneurysms involving the thoracic and abdominal aorta)
Complex aneurysms have a higher risk of complications or death. There were 63 active vascular units that reported complex AAA repairs to the NVR between 2019 and 2021. One unit performed 250 complex repairs during that time, but 34 units performed fewer than 20 procedures in the same interval.
In 2019-2021, there were 2123 procedures, of which 248 were open repairs.
The numbers have fluctuated over recent years with 803 procedures in 2019, 643 in 2020 and 677 in 2021. This represents a reduction around 16% between 2019 and 2021.
Among the 1875 endovascular procedures performed during the audit period, there were: 1073 fenestrated repairs (FEVAR), 152 branched repairs (BEVAR), 393 thoracic repairs (TEVAR) and 211 iliac branched grafts.
Rates of postoperative mortality after complex endovascular repairs were lower than after complex open repairs, being 2.6% for endovascular procedures (2.6% for FEVAR and 3.1% for TEVAR) and 10.9% for open repairs.
For open repairs, over 50% of patients were admitted to a level 3 critical care unit. The median overall postoperative stay was around 9 days. For endovascular repairs, most patients were admitted to level 2 critical care and the median length of stay was 4 days.
There was a total of 274 repairs for aortic dissection in 2019-2021. The overall mortality rate was 9.5% (7.3% for elective admissions and 11% for non-elective admissions).
Interestingly, 7.5% of patients were readmitted within 30 days following EVAR, compared with 5.7% following OR.
The level of case-ascertainment for these procedures is currently unknown because the coding of complex aortic procedures in the national administrative hospital datasets prevents these procedures from being clearly identified.
Repair of ruptured abdominal aortic aneurysms
During the audit period (Jan 2019- ec 2021) covered in the NVR report, details of 1,690 procedures were submitted to the NVR.
In the 2015 NVR Annual Report, open repairs constituted 78% of all procedures. Since then, the choice of EVAR has increased over time; in 2021, about 40% of patients with ruptured AAA underwent EVAR.
For ruptured endovascular aneurysm repair, general anaesthesia was used in 49.3% of cases compared to 47.25% for local anaesthetic alone and 2.51% for neuraxial anaesthesia.
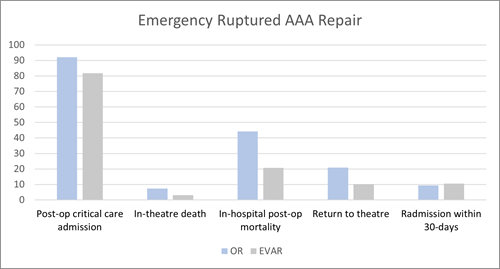
The in-hospital postoperative mortality rates for EVAR and open repair were 20.7% and 44.2%, respectively, in 2019-2021. We caution against comparing the figures for EVAR and open repair because patients who have open procedures may represent the more complex cases that are unsuitable for endovascular repair. We are also unable to comment on out-of-hospital care, such as transfers of patients from non-arterial hospitals to arterial hospitals.
The non-risk adjusted mortality rate after endovascular repair under local anaesthetic alone was 18.3%, compared to 20.8% for general anaesthesia alone.
All NHS trusts demonstrated in-hospital mortality rates after repair for ruptured AAA within the expected range, around the overall national average (35.3%).
Major Recommendations:
- Improve access to EVAR for emergency AAA via network-based pathways, access to hybrid facilities 24/7 and surgical/radiology workforce planning.

Lower Limb Interventions for Peripheral Artery Disease
1) Lower limb bypass
A total of 12,326 lower limb revascularisation procedures for chronic limb threatening ischemia (CLTI) (endovascular, hybrid and open bypass) were performed in 2021, which is slightly up from the previous year of 12,000, but significantly lower from 2019, when a total of 15,260 procedures were performed. Case ascertainment has remained stable over time for all procedures.
- A total of 3,149 elective open (bypass/hybrid) procedures were performed in 2021. This is a 10% increase from 2020 (n=2,864).
- There has been a small increase in the number of non-elective cases in 2021 (n=2,668), compared to 2020 (n=2,537).
- Majority of patients were over the age of 60 years presenting for elective and non-elective procedures, 81.3% and 80.2% respectively.
- With regards to type of anaesthesia for open surgery:
- 84.8% were performed under general anaesthetic
- 12.9% were performed under regional anaesthetic
- 2.3% were performed under local anaesthetic
- There was an increase in open surgical procedures for CLTI in 2021 (n=3,917) compared to 2020 (n=3,483).
- In 2021, 1,891 (48.3%) were admitted non- electively, a slight proportional decrease compared to 2020 (50.0%), indicating the resumption of elective activity in 2021
- 92.8% (n=5370) of open procedures (elective 98% and non-elective 86.7%) were performed between 8am and 6pm on a weekday. The percentage of open surgical procedures performed on planned lists was at least 75% for all but two NHS trusts that submitted 10 or more procedures in the NVR in 2021 (62 out of 64 NHS trusts, 96.9%)
- Most had comorbidities, the commonest being hypertension (66.4% elective, 65.6% non-elective), followed by ischaemic heart disease (30.9% elective, 33.9% non-elective) and diabetes (37.5% elective, 43.2% non-elective). A small proportion of patients had no comorbid disease (12.2% elective, 11.6% non-elective)
- 84.21% of elective patients and 77.3% of non-elective patients were recorded as being on one anti-platelet agent
- 82.47% of elective patients and 76% of non-elective patients were recorded as being on a statin
- Timing to revascularisation for chronic limb threatening ischaemia:
- Median wait from admission to intervention was 5 days (IQR 2-8 days) in 2021, compared to 4 days (IQR 2-8 days) in 2020
- 54.4% of non-elective bypasses were performed within 5 days of admission (the PAD QIF standard). This is lower than 2020 (59.6%) but higher than in 2019 (47%).
- A further procedure was required in 9% of elective admissions and 20.1% of non-elective admissions
- The length of stay was 5 days (IQR 3-8) for elective procedures and 14 days (IQR 8-24) for non-elective procedures
- Complications were relatively uncommon: 80.9% of elective and 78.9% of non-elective procedures did not require a further unplanned intervention
The In-hospital postoperative mortality rate was 1.3% for elective patients and 4.8% for non-elective patients.
The report highlighted that all NHS trusts risk adjusted in-hospital mortality following lower limb bypass has remained the same at 2.8% (95% CI: 2.5 to 3.0) in this cycle.
The anaesthetic technique information was extracted. This showed 84.8% of procedures were done under GA, 12.9% were performed under RA and only 2.3% were under LA. This is consistent with previous data and numbers are not large enough to show an impact on outcome.
Major Recommendations:
- Patients admitted with critical limb ischaemia as non-elective should have a
revascularisation procedure within 5 days
- Improved data entry for this group especially for those who require a second unplanned procedure during the same admission
2) Major lower limb amputation
There were 3,068 major unilateral lower limb amputations performed between January 2021 and December 2021: 49.9% (n=1,532) below-knee amputation (BKA) and 50.1% (n=1,536) above-knee amputation (AKA). Through knee amputation (TKA) accounted for 3.4% of cases and have been analysed as part of the BKA group. There has a been a slight reduction in the number of cases of unilateral amputations performed in 2021, compared to 2020 and 2019. The estimated case ascertainment for major unilateral lower limb amputations has remained stable, and the overall level exceeds the target of 85% recommended within the 2018 GIRFT vascular surgery report.
- BKAs were more common in those under the age of 60 (31.3%), while AKAs were more common in those over the age of 80 (23.4%). Most patients in both groups were mainly men, and were either current or ex-smokers
- More than 90% of patients had one or more comorbidities. Most patients requiring a BKA were diabetic (67.9%), compared to the majority being hypertensive (62.3%) in those requiring an AKA.
- It was common for patients to be on multiple medications, with antiplatelet agents, statins, antibiotic and DVT prophylaxis being the commonest.
- Oral anticoagulants were taken by 19-20% of patients
- Most patients were non-elective admissions and > 84% underwent surgery during daytime hours
- A consultant was present in > 70% of cases, however, this did not relate to the severity of the ASA assessment. Consultant presence for AKA was slightly lower (71.8% compared to 72.8% for BKA)
- Prophylactic antibiotics were recorded in 83% of procedures, and DVT prophylaxis was recorded in 72% of procedures. This may not reflect actual clinical practice but failure of data entry
- More than 25% of patients suffered one or more complication following major limb amputation; these were commonly respiratory (6.5% BKA, 8.9% AKA), cardiac (3.3% BKA, 4.4% AKA) and surgical site infections (4.8% BKA, 3.8% AKA). The proportion of cardiac complications were smaller in 2021 compared to 2019 (4.1% BKA, 6.2% AKA). A reduction in the rate of respiratory complications was seen compared to 2020; 8.0% for BKAs and 11.3% for AKAs
- 9.3 % BKA and 5.1% AKA had a return to theatre during their admission
- Most patients returned to the ward following an amputation, while 12% of BKA and 18% of AKA patients were admitted to critical care (level 2 or 3)
- The overall median length of hospital stay for major lower limb amputation was 21 days (IQR: 13 to 34 days)
- Adjusted 30-day mortality for all NHS trusts fell within the expected range from the national average of 6.6%
Anaesthetic data showed 46.71% of procedures were done under GA, 19.92% were combined GA with LA/RA and 33.38% were under LA/RA alone.
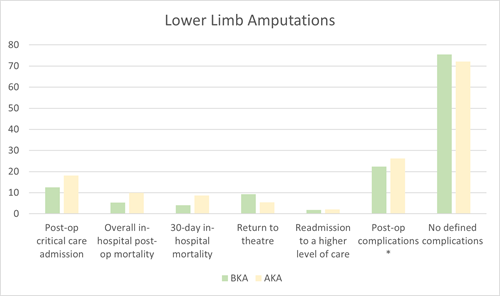
*Post-op complications include respiratory, cardiac, limb ischaemia, renal failure, surgical site infection, post-operative confusion, haemorrhage, cerebral
Major Recommendations:
- Patients for major amputation should be admitted to a recognised arterial centre via agreed time-based protocols
- Patients admitted non-elective for critical limb threatening ischaemia should have their revascularisation surgery within 5 days
- A consultant should be present or at least supervising a senior trainee (ST4 and above) undertaking the amputation
- The patient should have routine antibiotic and DVT prophylaxis according to local policy and this should be recorded on NVR
- Ensure access to a specialist amputee rehabilitation team including psychological support
Dr Katie Ayyash and Dr Elisa Dedola
VASGBI Research & Audit Committee
